ITPC’s Global Survey on Access to and Quality of HIV Treatment and Care focused on barriers to quality HIV care and treatment across 14 low- and middle-income countries covering seven regions of the world.
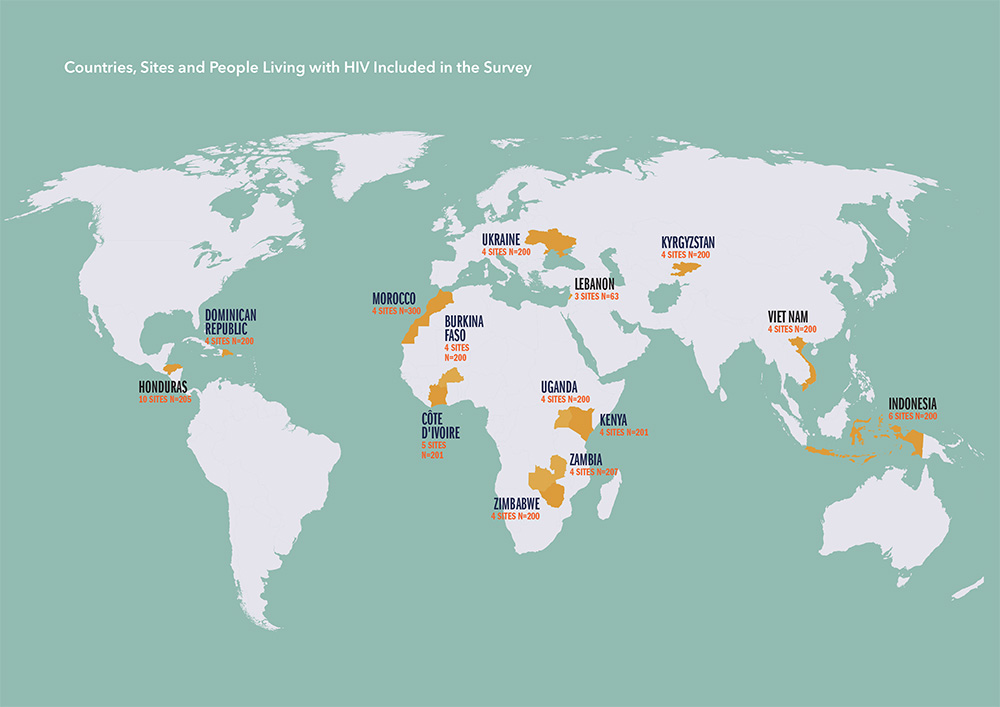
The peer-led research was conducted between April and December 2018 as part of the Watch What Matters campaign.
The survey and resulting report has identified access barriers and gaps, along with poor quality of services, experienced by people living with HIV. Despite progress in the global HIV response, it remains the case that in many countries, the average person living with HIV still faces crippling blockages to treatment. As of 2018, only 62% of the world’s 37.9 million people living with HIV were accessing antiretroviral therapy (ART).
As of 2018, only 62% people living with HIV were accessing treatment.
 The data highlighted a number of key barriers including stigma and discrimination, which continues to be a persistent and deadly barrier to treatment access, with an overwhelming number of recipients of care only presenting at clinics when they are gravely ill. Nearly half (47.7%) of survey participants were tested for HIV because they were ill.
The data highlighted a number of key barriers including stigma and discrimination, which continues to be a persistent and deadly barrier to treatment access, with an overwhelming number of recipients of care only presenting at clinics when they are gravely ill. Nearly half (47.7%) of survey participants were tested for HIV because they were ill.
The results also underlined the critical need for treatment education along the continuum of care. People living with HIV must be able to make informed choices in order to fully access their right to health.
Other barriers included people being prescribed sub-optimal treatment; a lack of affordable, optimal medicines; issues affecting adherence; and a lack of viral load (VL) testing or VL results being acted upon.
The research also found that any ART centres do not have the capacity to diagnose and/or treat recipients of care for opportunistic infections. Tuberculosis (TB), although preventable and curable, is the leading cause of death among people living with HIV. The WHO recommends screening periodically for TB, yet only 77.1% of survey participants reported being asked about symptoms and whether they had had recent contact with a person who had TB.
All of these barriers undermine the success of global efforts to end AIDS.
Best way to remove barriers
A main finding of the survey is that community-led approaches empower the beneficiaries of HIV treatment to monitor and improve the quality of healthcare that they receive.
“We can’t change the game if we keep doing business as usual; we need to put the money where the evidence is” says Solange Baptiste, ITPC Executive Director.
Summary of recommendations
Based on the findings of the study, ITPC recommends the following key steps to be taken to improve access to and quality of HIV services, which will bring the world closer to ending AIDS. You can read the recommendations and report in full here.
- PROVIDE TREATMENT EDUCATION to recipients of care and healthcare workers, essential for supporting adherence, particularly with the advent of ‘treat-all’, as more people who are asymptomatic are diagnosed and initiated on ART.
- SCALE-UP DIFFERENTIATED SERVICE DELIVERY to improve access to culturally competent HIV care, treatment and support services based on the needs of recipients of care.
- EXPAND VIRAL LOAD TESTING including prompt delivery of results and indicated actions, through decentralized point of care testing viral load testing.
- PROVIDE FULLY INTEGRATED HEALTHCARE CARE without user fees, through the co-location of screening and treatment services.
- IMPLEMENT COMMUNITY TREATMENT OBSERVATORIES (CTOs) to improve access to quality and consistent supply of HIV services, treatment and commodities through community-led monitoring mechanisms.
- MAINTAIN BASELINE CD4 TESTING (and monitoring, when indicated), to identify people who are presenting or returning to care with advanced HIV.
- INCREASE SUPPORT FOR AND BREADTH OF COMMUNITY-LED APPROACHES, to increase linkage to and engagement in HIV services.
- PROMOTE THE RIGHTS OF PEOPLE LIVING WITH HIV and key populations, through rights-based approaches.
- MAKE MEDICINES AFFORDABLE. Ensure that WHO- recommended, optimal treatment regimens are available and affordable everywhere, by addressing intellectual property and regulatory barriers to market entry of generic products, and by increasing competition between generics producers.




